Imagine if it became more difficult every time you went to unlock your front door. The key began to stick and required some jiggling, eventually not working at all. Well, that’s ok, you’ve got a spare key. It works at first, but over time the same problem happens. Next, you probably need another key, then another, and another. And the cycle continues until you have a ton of keys that aren’t opening the door. Great.
Diabetes is a condition where your body doesn’t regulate blood sugar appropriately. Type 2 diabetes has become increasingly common, especially in developed countries. Over 10 percent of Americans have diabetes, and 1 in 5 do not know they have it. One-third of the US population has pre-diabetes, and 8 in 10 are unaware. Diabetes is the seventh leading cause of death in the United States and the leading cause of kidney failure, adult blindness, and lower-limb amputation.
Why is diabetes so common? What is the pathology behind this disease? And most importantly, how do I prevent or treat it, so I don’t become a statistic?
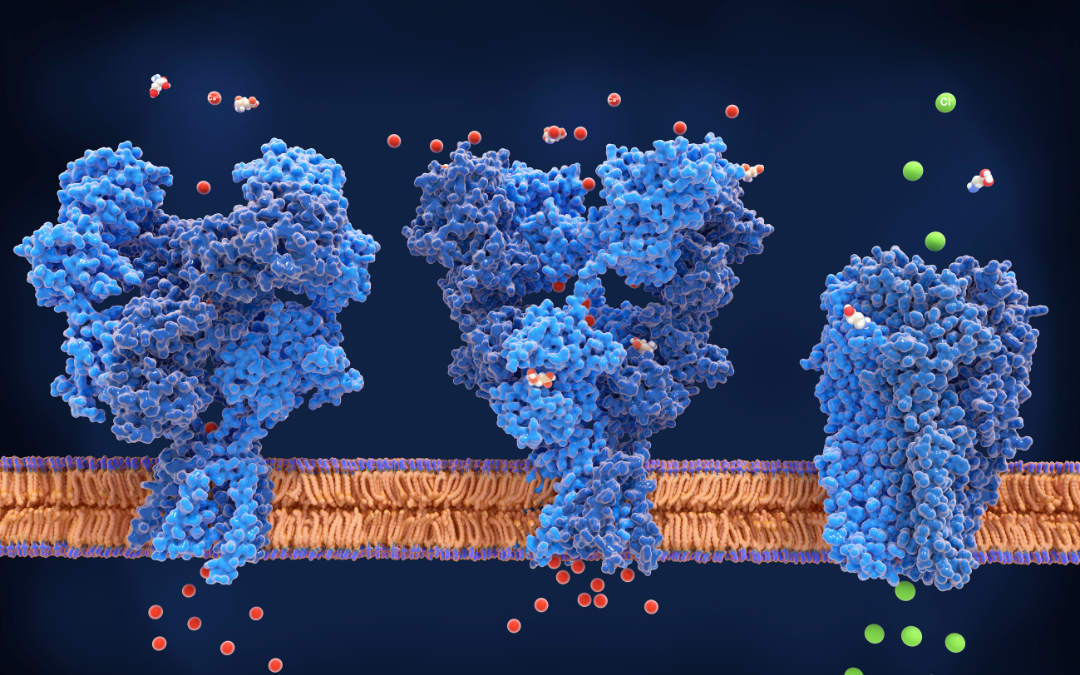
Let’s review the usual mechanism of how glucose, or sugar, is shuttled into our cells. First, upon digestion of food containing sugar or carbohydrates, our pancreas releases the hormone insulin. Insulin acts as a key, opening the door and letting glucose into our cells. These cells get the energy they need, and our blood sugar remains stable. All is well.
Diabetes is driven by a mechanism known as insulin resistance. It occurs when your body’s cells no longer listen to insulin as it’s trying to unlock the door and put glucose inside the cells. The key is no longer working. The pancreas gets the signal and makes more insulin (more keys! All we need is more keys!). Eventually, though, insulin cannot keep up, and there is a rise in blood glucose. If this process continues, what began as insulin resistance results in pre-diabetes and eventually type 2 diabetes.
This process doesn’t happen overnight. It typically takes years to progress into overt diabetes, and most people don’t realize they are heading in that direction. That’s why monitoring your glucose and checking fasting insulin with routine labs are essential. At Integrative Family Medicine of Asheville, practitioners listen to your personal and family history to determine the specific labs that will provide helpful information for your overall health. With a family history of diabetes, periodic monitoring will provide insight into whether your insulin is starting to rise. When this happens, your cells change the locks (insulin resistance!).
There are many nuances not discussed here, as glucose is not the only fuel for your cells, and some cells may prefer fat or ketones. The difficulty is that when your body prefers sugar for fuel, you may lose the ability to burn fat. Insulin inhibits the cells from releasing fat for fuel. This inflexibility can present as hypoglycemia if you don’t keep up with regular sugar intake.
It’s vital to have metabolic flexibility. This flexibility allows you to use both energy sources as needed depending on what’s available and prevent insulin resistance and diabetes. Here are some ways to guide your metabolism in the right direction:
Eating Strategy:
Include a variety of vegetables, especially colorful vegetables, which are loaded with antioxidants and phytonutrients. These properties help reduce inflammation and nurture the gut microbiome. Limiting or avoiding high glycemic index foods can help reduce blood glucose and insulin levels. Insulin can be inflammatory when chronically elevated and perpetuates the process of developing insulin resistance and overt diabetes.
Movement:
Resistance training is a great way to increase glucose uptake in our muscles. Compound movements like squats and deadlifts are great when done safely. It’s best to consult a trainer or physical therapist if these movements are new to you. High-Intensity interval training is an efficient way to promote muscle growth AND work the cardiovascular system.
Stress Management:
The stress hormone cortisol increases our blood glucose level, so managing stress is essential. Stress management can take many different forms, the most recognizable being meditation. Here are some other things that help with stress: listening to music, walks in nature, art, deep breathing, and exercise.
Sleep:
7-8 hours of sleep is critically important to regulate key hormones, including cortisol and insulin. These hormones, along with others, help control appetite, weight, and immunity. Reduced sleep contributes to insulin resistance. Sleep is non-negotiable in the discussion around chronic disease prevention, including diabetes.
Preventing and treating diabetes is complicated. A healthy eating strategy and lifestyle are essential, and this looks different for everyone. The current food environment makes it challenging to be successful, especially long-term. An integrative health coach can help develop a plan that works for you as an individual.
If you are concerned about insulin resistance or diabetes and are looking for a different approach, reach out to an integrative family medicine clinic. Here, you will find the space to explore the “why” behind chronic disease. We are here to help guide you toward optimal health, whatever that means to you.
Disclaimer: The cellular mechanisms in this post are distilled to the point of being comedic. Our bodies are complicated! For more information, please proceed to the nearest university biology lab.
References:
1. Research and Statistics
2. www.cdc.gov
3. Petersen MC, Shulman GI. Mechanisms of Insulin Action and Insulin Resistance. Physiol Rev. 2018 Oct 1;98(4):2133-2223. doi: 10.1152/physrev.00063.2017. PMID: 30067154; PMCID: PMC6170977.
This post was written by Integrative Family Medicine of Asheville’s Thomas Everts, PA-C.