As we head into Breast Cancer Awareness month, we thought it would be a good time to review the data and statistics around breast cancer in this country, including rates of breast cancer diagnosis, screenings, outcomes and risk factors associated with the development of breast cancer. If you read through this post and have more questions, please feel free to reach out to your Integrative Family Medicine provider so we can help you navigate your questions and personal risk.
Breast cancer stats in the United States
-
- Breast cancer remains the most common cancer and the second leading cause of cancer death among women in the United States. (Lung cancer is first, and pancreatic/colon follow breast cancer).
- Estimated lifetime risk of diagnosis is 1 in 8 (13.1%). The lifetime risk of death is 1 in 43 (2.3%).
- In 2024, approximately 310,720 new cases of invasive breast cancer and 42,250 deaths were expected among women. Incidence rates have increased by about 1% annually over the past decade, with higher rates among women under 50. Notably, Black women have a 38% higher mortality rate than White women, highlighting disparities in access to early diagnosis and treatment. [1,2]
Risk Factors
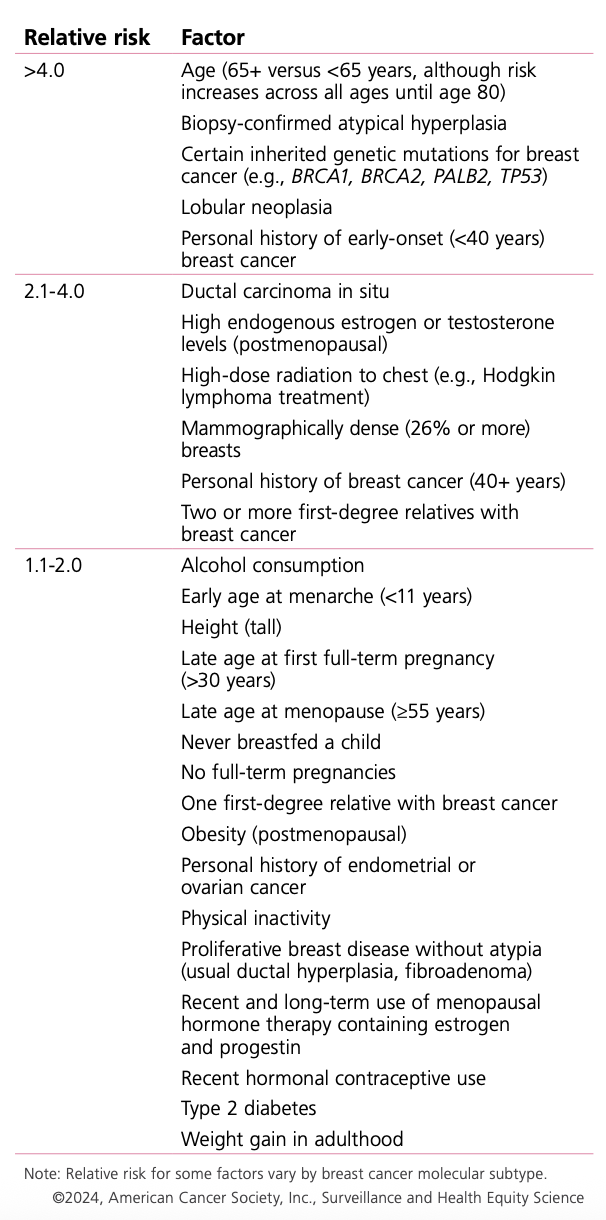
Risk factors are things that increase the risk of breast cancer diagnosis. There are 2 types: modifiable (meaning things we can change about our habits, environment or lifestyle) and nonmodifiable (things we cannot change about our genetics or makeup). Approximately 30% of cases can be attributed to potentially modifiable risk factors!
Modifiable risk factors include:
-
-
- Healthy weight (obese patients have a higher rate of diagnosis)
- Regular physical activity (more active patients have lower rates of diagnosis, where more sedentary patients tend to have higher diagnoses)
- Alcohol intake (increased alcohol consumption is linked with an increased risk of diagnosis)
- Smoking tobacco (similar to alcohol, tobacco users have higher rates of breast cancer diagnosis)
-
Nonmodifiable risk factors include:
-
-
- Prior history of breast cancer*
- History of dense breast tissue or abnormal breast tissue*
- Positive for BRCA1 or BRCA2 gene*
- Family history of breast cancer
- Increasing age
- Recent and long term use of birth control or hormone therapy that includes estrogens and progestins
- Early menarche (<11) or late onset menopause (>55)
- No history of breastfeeding or carrying full term pregnancy
-
*these are the three strongest risk factors for the development of breast cancer [3]
Table 3. Factors that Increase Risk of Invasive Female Breast Cancer
Diagnosis
-
- Screening exams (testing for a disease before signs and symptoms develop) are designed to detect breast cancers early to allow for less treatment and better outcomes. Diagnostic exams (testing for a disease after signs or symptoms develop) are also an important part of breast cancer diagnosis, but often reflect a more advanced stage of breast cancer.
- A mammogram is a special breast X-ray that can find cancer early, sometimes before you can feel it. Your breast is gently pressed between two plates for a few seconds to get a clear picture, and then the images are read by a radiologist who has specialization in reading and interpreting breast studies.
- Different organizations in the United States have slightly different recommendations for when to start screening with mammography:
| Organization | Recommended Start Age | Frequency | Notes |
|---|---|---|---|
| USPSTF (U.S. Preventive Services Task Force) | 40 | Every 2 years (biennial) | Continue through age 74; moderate certainty of moderate net benefit |
| ACS (American Cancer Society) | 45 (option to start at 40) | Annual ages 45–54; every 2 years from 55+ | Screening may continue as long as woman is in good health |
| ACOG (American College of Obstetricians and Gynecologists) | Offer from 40 | Every 1–2 years | Shared decision-making on frequency; continue after 75 based on health status |
- The primary benefit of mammography is a reduction in breast cancer mortality, estimated at 20–30% depending on age and screening interval. However, screening also carries risks: false positives (leading to anxiety and unnecessary biopsies), overdiagnosis (detection of cancers that would not have become clinically significant), and cumulative radiation exposure. [3]
- Surprisingly, clinical breast examination and breast self-examination are not recommended for average-risk women due to lack of mortality benefit and increased false positives, though many patients and providers prefer to do them. For patients at high-risk, manual breast exams are reasonable to perform.
- Sometimes, if a patient is at higher risk for the development of breast cancer, additional kinds of tests can be included in screening such as ultrasound of the breast, the addition of iodinated contrast during the mammogram or breast MRIs. Some of these tests are also used in diagnostic exams.
In summary, breast cancer screening saves lives but requires individualized, shared decision-making to balance benefits and harms. Addressing lifestyle factors and ensuring equitable access to screening and treatment are essential for reducing the burden of breast cancer.

This blog post was written by Liz Frost, PA-C, MSCP and Vice President at Integrative Family Medicine of Asheville. You can read more about Liz in her bio.
References
1. Breast Cancer Facts & Figures.
Gladys Arias, Steve Bouvier, Christy Cushing, et al
American Cancer Society (2025)
Practice Guideline
2. Breast Cancer Statistics, 2022.
Giaquinto AN, Sung H, Miller KD, et al.
CA: A Cancer Journal for Clinicians. 2022;72(6):524-541. doi:10.3322/caac.21754.
Leading Journal
4. Screening for Breast Cancer: US Preventive Services Task Force Recommendation Statement.
Nicholson WK, Silverstein M, Wong JB, et al.
JAMA. 2024;331(22):1918-1930. doi:10.1001/jama.2024.5534.
Practice Guideline
Leading Journal

