Cholesterol 101: Making Sense of LDL, HDL, Triglycerides, and Beyond
You know that moment when you get your cholesterol results back and suddenly feel like you need a medical degree just to understand what you’re looking at? You’re not alone. Between conflicting advice on the internet, your well-meaning friend who swears by their ketogenic diet, and that one podcast episode you half-listened to while doing dishes, cholesterol has become one of the most confusing topics in health and wellness.
Let’s clear things up.
The Standard Lipid Panel: Your Starting Point
When your doctor orders a “lipid panel” or “cholesterol test,” you’re typically getting five key measurements:
Total Cholesterol– This is exactly what it sounds like: the sum of all cholesterol in your blood. While it gives a quick snapshot, it’s a bit like knowing the total number of cars on the highway without knowing which direction they’re heading or how fast they’re going.
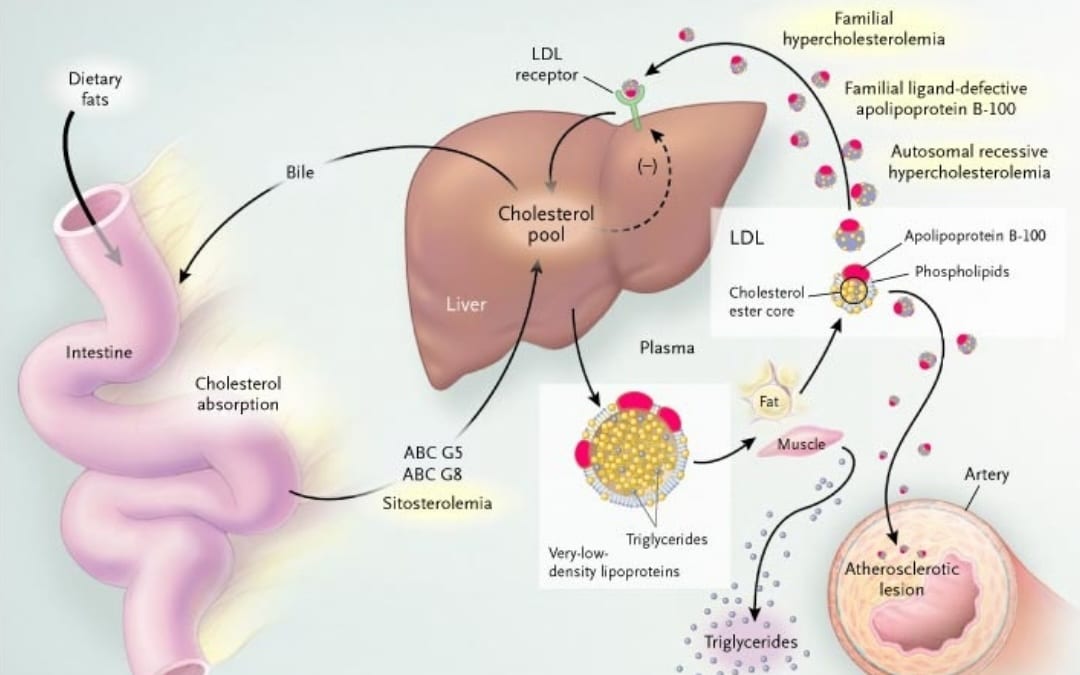
LDL Cholesterol (Low-Density Lipoprotein)– Often called “bad cholesterol,” though that’s oversimplified. LDL particles are like delivery trucks carrying cholesterol through your bloodstream. The problem isn’t the cholesterol itself—your body needs it for making hormones, cell membranes, and vitamin D. The issue is when these particles get stuck in your arterial walls.
VLDL Cholesterol (Very Low-Density Lipoprotein)– The triglyceride-heavy cousin of LDL. These are the supersized delivery trucks carrying more fat than cholesterol.
Triglycerides– These are the actual fat molecules in your blood, mainly reflecting what you’ve recently eaten and how your body processes carbohydrates and fats.
HDL Cholesterol (High-Density Lipoprotein)– The so-called “good cholesterol.” These particles act like garbage trucks, picking up excess cholesterol from your arteries and hauling it back to the liver for disposal.
What These Numbers Actually Tell Us About Heart Disease Risk
Here’s where the science gets interesting—and where the standard panel, while useful, only tells part of the story.
The ApoB Story: It’s About the Particles, Not Just the Cholesterol
Research has definitively established that ApoB particles cause atherosclerosis—the buildup of plaque in arteries that leads to heart attacks and strokes. But here’s the nuance: It’s not simply the cholesterol concentration in blood that matters, but the number of ApoB-containing particles delivering cholesterol into the artery wall.
ApoB particles are small enough (under 70 nanometers), allowing them to slip through the arterial wall and get trapped in the space beneath. Once there, the particle and the cholesterol they were carrying are treated as a foreign body–—think of it as a splinter in your finger. When you get a splinter, your body creates an inflammatory response around it. Similarly your body creates an inflammatory response around the ApoB particle, creating a “plaque” This plaque formation can eventually restrict blood flow or rupture, causing acute cardiac events.
The critical insight from decades of research involving over 2 million participants is this: the number of ApoB particles matters more than the amount of cholesterol they carry. Your standard cholesterol panel measures LDL cholesterol (LDL-C), which is an estimate of how much cholesterol is in those particles—but it doesn’t tell you how many particles you have.
Triglycerides: The Inflammatory Wildcard
Elevated triglycerides deserve more attention than they typically get. When triglyceride-rich lipoproteins get broken down, they create smaller remnant particles that are particularly good at penetrating arterial walls. Recent evidence suggests these remnants might be even more atherogenic than LDL particles on a per-particle basis.
What makes triglycerides especially problematic is their inflammatory effect. Unlike LDL, which contributes to heart disease primarily through physical accumulation, elevated triglyceride remnants are causally associated with both cardiovascular disease andsystemic inflammation. Studies show that nonfasting triglycerides of 580 mg/dL compared to 70 mg/dL confer a 5-fold increased risk for heart attack.
HDL: When “Good Cholesterol” Gets Complicated
For years, we thought higher HDL was always better—but the story is more nuanced. HDL’s primary protective mechanism is reverse cholesterol transport: pulling cholesterol out of arterial plaques and delivering it to the liver for elimination. HDL also has anti-inflammatory and antioxidant properties that protect against atherosclerosis.
However—and this surprised researchers—simply having high HDL cholesterol doesn’t guarantee protection. Studies now show a U-shaped relationship between HDL levels and mortality, with very high levels (above 80 mg/dL in men, 100 mg/dL in women) actually associated with increased cardiovascular risk. Additionally having a low HDL is thought to be a signal for metabolic syndrome.
The issue is that HDL cholesterol measures quantity, not quality or function. Under conditions like diabetes, chronic inflammation, or established heart disease, HDL can become dysfunctional—losing its protective properties and potentially becoming pro-inflammatory. It’s HDL’s function—specifically its ability to remove cholesterol from cells—that matters for cardiovascular protection, not just the number on your lab report.
Beyond the Basics: Advanced Lipid Testing
The standard lipid panel is accessible, affordable, and provides valuable screening information. But if you want a more detailed picture of your cardiovascular risk—especially if you have a family history of early heart disease, diabetes, or metabolic syndrome—consider these advanced markers:
Apolipoprotein B (ApoB)– This directly measures the number of atherogenic particles in your blood. Every LDL, VLDL, and remnant particle contains exactly one ApoB protein, making it a precise count of all the potentially harmful particles. Many consider this the single best lipid marker for cardiovascular risk.
Lipoprotein(a) or Lp(a)– A genetic variant of LDL that’s independently associated with increased cardiovascular risk. Unlike other lipid markers, Lp(a) isn’t significantly affected by diet or most medications, and elevated levels affect about 20% of the population. When elevated, this can increase a person’s risk of a cardiovascular event by 2-3 fold.
High-Sensitivity C-Reactive Protein (hs-CRP)– Measures inflammation in your body. Since atherosclerosis is fundamentally an inflammatory disease, knowing your inflammatory status adds important context to your lipid numbers.
LDL Particle Number (LDL-P) and LDL Size– Directly measures how many LDL particles you have and whether they’re the smaller, denser (more dangerous) type or larger, fluffier particles.
The Bottom Line
Your standard cholesterol panel is a valuable screening tool that’s affordable and widely available. It gives important information about your cardiovascular risk and helps guide clinical decisions.
But remember: those five numbers are measuring proxies—estimates based on cholesterol content—rather than the underlying biology of atherosclerosis. When discussing metabolic health, understanding the mechanism behind the measurements helps us make better decisions about our health.
If you’re at higher risk or want a more comprehensive picture, advanced lipid testing can provide critical additional information. The key is working with a healthcare provider who understands both the value and the limitations of each test, and who can help you interpret your results in the context of your overall health picture.
After all, the goal isn’t just to optimize numbers on a lab report—it’s to understand your individual cardiovascular risk and, ultimately, to live a longer, healthier life.
If you have questions about your cholesterol panel or want to explore advanced lipid testing options, our team at Integrative Family Medicine of Asheville is here to help you understand your cardiovascular risk and develop a personalized approach to your heart health. Schedule a consultation with one of our providers to discuss how we can work together to optimize your metabolic wellness.

This blog post was written by Chad Krisel, Co-Founder and CEO of Integrative Family Medicine. You can read more about Chad in his bio.
References
LDL and Atherosclerosis:
- Cardiovascular Disease.The New England Journal of Medicine. 2003. Nabel EG. (image)
- Ference BA, Ginsberg HN, Graham I, et al. Low-Density Lipoproteins Cause Atherosclerotic Cardiovascular Disease. 1. Evidence From Genetic, Epidemiologic, and Clinical Studies. A Consensus Statement From the European Atherosclerosis Society Consensus Panel. European Heart Journal. 2017;38(32):2459-2472. doi:10.1093/eurheartj/ehx144.
- Borén J, Packard CJ, Binder CJ. Apolipoprotein B-Containing Lipoproteins in Atherogenesis. Nature Reviews Cardiology. 2025;22(6):399-413. doi:10.1038/s41569-024-01111-0.
- Ference BA, Graham I, Tokgozoglu L, Catapano AL. Impact of Lipids on Cardiovascular Health: JACC Health Promotion Series. Journal of the American College of Cardiology. 2018;72(10):1141-1156. doi:10.1016/j.jacc.2018.06.046.
- Pothineni NVK, Karathanasis SK, Ding Z, et al. LOX-1 in Atherosclerosis and Myocardial Ischemia: Biology, Genetics, and Modulation. Journal of the American College of Cardiology. 2017;69(22):2759-2768. doi:10.1016/j.jacc.2017.04.010.
Triglycerides and Remnants:
- Ginsberg HN, Packard CJ, Chapman MJ, et al. Triglyceride-Rich Lipoproteins and Their Remnants: Metabolic Insights, Role in Atherosclerotic Cardiovascular Disease, and Emerging Therapeutic Strategies-a Consensus Statement From the European Atherosclerosis Society. European Heart Journal. 2021;42(47):4791-4806. doi:10.1093/eurheartj/ehab551.
- Björnson E, Adiels M, Gummesson A, et al. Quantifying Triglyceride-Rich Lipoprotein Atherogenicity, Associations With Inflammation, and Implications for Risk Assessment Using Non-HDL Cholesterol. Journal of the American College of Cardiology. 2024;84(14):1328-1338. doi:10.1016/j.jacc.2024.07.034.
- Nordestgaard BG. Triglyceride-Rich Lipoproteins and Atherosclerotic Cardiovascular Disease: New Insights From Epidemiology, Genetics, and Biology. Circulation Research. 2016;118(4):547-63. doi:10.1161/CIRCRESAHA.115.306249.
- Raposeiras-Roubin S, Rosselló X, Oliva B, et al. Triglycerides and Residual Atherosclerotic Risk. Journal of the American College of Cardiology. 2021;77(24):3031-3041. doi:10.1016/j.jacc.2021.04.059.
HDL Function and Paradox:
- Pownall HJ, Rosales C, Gillard BK, Gotto AM. High-Density Lipoproteins, Reverse Cholesterol Transport and Atherogenesis. Nature Reviews Cardiology. 2021;18(10):712-723. doi:10.1038/s41569-021-00538-z.
- Linton MF, Yancey PG, Tao H, Davies SS. HDL Function and Atherosclerosis: Reactive Dicarbonyls as Promising Targets of Therapy. Circulation Research. 2023;132(11):1521-1545. doi:10.1161/CIRCRESAHA.123.321563.
- Razavi AC, Jain V, Grandhi GR, et al. Does Elevated High-Density Lipoprotein Cholesterol Protect Against Cardiovascular Disease? The Journal of Clinical Endocrinology and Metabolism. 2024;109(2):321-332. doi:10.1210/clinem/dgad406.
- Rosenson RS, Brewer HB, Ansell BJ, et al. Dysfunctional HDL and Atherosclerotic Cardiovascular Disease. Nature Reviews Cardiology. 2016;13(1):48-60. doi:10.1038/nrcardio.2015.124.