Direct Primary Care in 2026: From Fringe Idea to Proven Model
For years, Direct Primary Care (DPC) was considered an “alternative” approach to healthcare. As of 2026, it’s clear that DPC has entered a new phase—mature, established, and increasingly mainstream.
Across the country, patients, physicians, and employers are turning to DPC because it restores something healthcare has largely lost: time, access, and relationship.
Here’s what’s happening in the DPC world—and why it matters.
DPC by the Numbers: A National Movement
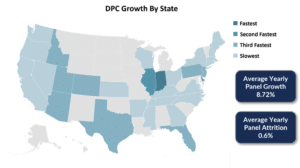 As of early 2026, there are nearly 3,000 verified DPC clinics operating across the United States—up from about 2,000 just a few years ago. DPC practices now exist in all 50 states, with strong growth in places like North Carolina, Texas, and Florida.
As of early 2026, there are nearly 3,000 verified DPC clinics operating across the United States—up from about 2,000 just a few years ago. DPC practices now exist in all 50 states, with strong growth in places like North Carolina, Texas, and Florida.
This growth isn’t random. It reflects rising frustration with insurance-based care and a growing demand for healthcare models that are simpler, more transparent, and more human.
Why DPC Doctors Can Spend More Time With Patients
One of the defining features of DPC is smaller patient panels.
The average DPC physician cares for about 400 patients
Most aim for a full panel of 500–600 patients
In contrast, traditional primary care doctors often manage 2,300–2,500 patients
This difference is everything. Smaller panels allow DPC physicians to offer 30–60 minute appointments, same-day or next-day access, and real continuity of care. Instead of rushing through visits, doctors can focus on prevention, chronic conditions, and long-term health goals.
Big Shifts Shaping DPC in 2026 and Beyond
1. DPC Is Now HSA-Eligible
As of January 1, 2026, federal guidance clarified that DPC membership fees can be paid using Health Savings Accounts (HSAs). This removes a long-standing barrier and makes DPC more accessible for individuals and families who rely on tax-advantaged healthcare dollars.
2. Smaller, More Flexible Clinics
Many DPC physicians are opening “micro-practices”—using shared spaces or mobile setups to keep overhead low. Some clinics can now sustainably operate with as few as 150 patients, making DPC viable in rural and underserved areas.
3. Employers Are Driving Growth
More than half of all DPC growth is now driven by small and mid-sized businesses. Employers are increasingly offering DPC memberships directly to employees, often paired with high-deductible or catastrophic insurance plans.
For employers, this approach means:
Lower and more predictable healthcare costs
Happier, healthier employees
Fewer missed workdays due to delayed care
DPC as a “Longevity Hub”
Because DPC isn’t restricted by insurance billing rules, many practices are expanding services focused on long-term health and prevention, including:
Health coaching for nutrition, sleep, and stress
Advanced lab testing to personalize care
Longer, more personalized visits
This flexibility allows patients to address health proactively rather than reactively.
The Bottom Line
Direct Primary Care isn’t a trend—it’s a structural shift in how healthcare is delivered.
By simplifying payment, reducing administrative burden, and prioritizing time and relationships, DPC offers a model that works better for patients, clinicians, and employers alike. As healthcare costs continue to rise and access becomes more fragmented, DPC is proving to be a durable, scalable alternative.
Learn more about DPC Membership at Integrative Family Medicine of Asheville here.


